Features
Summary
Findings
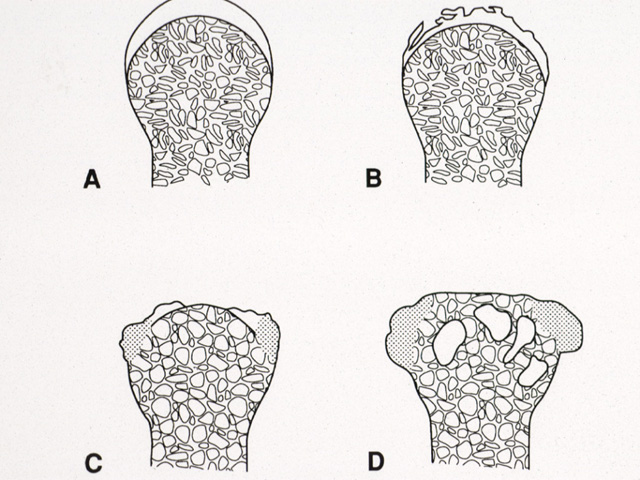
A. Normal architecture with intact cartilage. B. Degeneration of articular cartilage through fragmentation and thinning. C. Calcification of cartilage margins (shaded areas), and patchy loss of cartilage, exposing bare bone (eburnation). D. Formation of lips of new bone (osteophytes), extensive loss of cartilage, and cystic degeneration of underlying bone.
Impression
Osteoarthritis
Pathology Pointer
The fundamental feature of this disease is progressive loss of articular cartilage with reactive bone changes to stress, not inflammation. Mechanical wear, changes in chondrocyte function and matrix composition lead to cartilage loss. These changes interfere with the remodeling and maintenance of cartilage. Additional risk factors include repetitive mechanical effects or joint loading ("wear and tear”), obesity, joint injury, and inactivity. Thus, patients are encouraged to exercise because joint use provides adequate stimulation of chondrocyte activity and tissue remodeling in the non-cellular matrix. With loss of articular cartilage, exposure of underlying bone to weight-bearing forces triggers abnormal repair, leading to reactive bone changes such as osteophytes and sclerosis. Osteoarthritis is managed with anti-inflammatory medications, exercise, glucosamine, and intra-articular injections with steroid and/or hyaluronic acid. Definitive treatment is by arthroplasty, the replacement of the joint by a metal/polymer construct.
View
Sequence of development of osteoarthritis, diagram
Specimen
-
Image Credit
Katsumi M. Miyai, M.D., Ph.DDepartment of Pathology
School of Medicine
University of California, San Diego